57 countries have critical shortages in health care workers, with a total deficit of 2.4 million health professionals worldwide. A brief assessment of health statistics in the developing world reveals a picture of unnecessary tragedy.
Africa particularly is challenged with critical shortage of health workers, lack of health systems that enable communication between rural and urban centers and a big bottom of the pyramid population that are illiterate about basic health practices.
According to the World Health Organization (WHO), an estimated [21.6 million–25.5 million] people were accessing antiretroviral therapy (end of June 2019), and 2.5 million people were newly infected with HIV ; every minute, at least one woman dies from complications related to pregnancy or childbirth. In 2015, an estimated 303 000 women died from the same complications. And for every woman who dies in childbirth, around 12 more suffer injury, infection or disease—approximately 10 million each year. At the same time, communicable diseases such as malaria, yellow fever and cholera continue to claim lives due to preventable factors such as a lack of access to proper drugs and medical treatment. Looking beyond, HiPipo Foundation is committed to support WHO in accelerating reductions in preventable deaths by 2030, as part of the Sustainable Development Goals agenda.
A number of the diseases are preventable or treatable if affected parties have access to medical personnel and or to supportive communities for reliable information to prevent or manage these conditions. As such we currently working on two amazing eHealth and mHealth projects namely My Doctor and God Mother to help accelerate health care services in Africa.
My Doctor
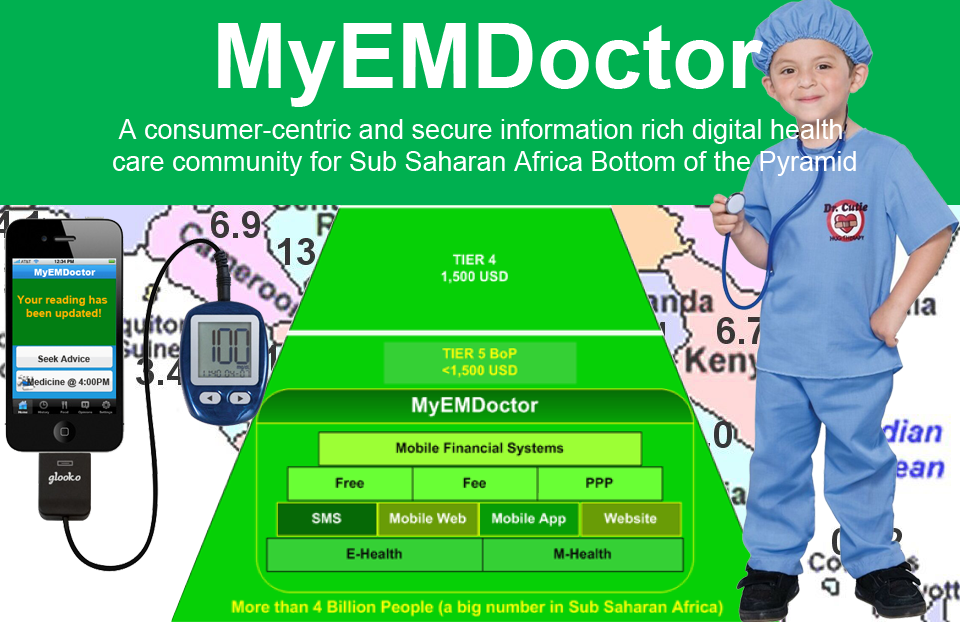
My eHealth and mHealth Doctor (My Doctor) is a project that takes a consumer centric approach to health, by offering a digital community that enables doctor to patient interaction together with patient to patient information sharing and later monitoring. The same digital community serves researchers and governments through reliable remote data gathering and aggregate research data.
With My Doctor, African unserved people can find reputable health centers, hospitals, clinicians and friends with common afflictions. The digital community helps African people who are looking to make an educated health care decision. My Doctor project deploys FREE, FEE and Public Private Partnership (PPP) business models to deliver eHealth and mHealth benefits to the Bottom of the Pyramid (BoP), while enabling interoperable and low-cost payment solutions to ensure access of the most required health care services anytime.

GodMother
GodMother; is a project that will bring mHealth access to the excluded bottom of the pyramid (BoP) women, families and healthcare providers in remote villages.
A God motherly approach aims at impacting populations by distributing responsibility and getting more people involved in ensuring that routine immunization of all infants is improved. This will see health workers, fathers, grandparents, sisters, brothers, close friends, in-laws and other family members get involved in ensuring that every child gets all required immunization. This God motherly approach will ensure that every child born has at least two next of kin sureties that will carry on the responsibility and be part of the reminding and monitoring circle of every child’s immunization.
In a world where digital financial services have brought financial inclusion to a tipping point, integrating social services with financial services at low-cost, seamless, real-time payments means deliberate and collaborative action across sectors. Our prayer is that God Mother solution through making use of interoperable open source solutions such as Mojaloop between digital financial services will help change the mindset of citizens to shift heavy expenditures of baby showers to helping other women have safe births and also help babies get collaborative care takers.
God Mother will help mothers get support and funding contributions from anyone anywhere in the world seamlessly.
The worldwide health challenges facing tens of millions of citizens, and especially children, present arguably the most significant barrier to global economic development and the SDGs agenda.
Fortunately new information and communication technologies (ICTs) are now available to help improve public health, with wireless communications being the most ubiquitous and widely accepted of these technologies within the developing world.
While there is no panacea to the complex and multifaceted challenges of improving public health outcomes, mHealth—existing at the nexus of the health and technology social domains—provides an extraordinary opportunity to bring about significant improvements.
It is so true, Mobile technology represents a high reach, cost-efficient method for making health care more accessible, affordable and effective across the developing world.
With 90% of the world’s poor now covered by a mobile signal, and the GSM Association (GSMA) expects that figure to improve, we have a unique opportunity to use low-cost digital tools to serve people who have been historically underserved, with new world mHealth solutions.
The annual assessments and reports of progress toward the Millennium Development Goals and UN Sustainable Development Goals (SDGs) state that mHealth has capacity to proliferate the speed at which the most required health requests are addressed in the developing world.
Indeed mHealth has tremendous potential to scale and provide dramatically improved health outcomes. With this, the efficiency of health care provision will significantly improve, and the health services provision will become more effective.
We want to lead the continents healthcare-focused investment activities in two ways, First; by developing low cost mHealth solutions that help create an incredible mobile health ecosystem that connects with all stakeholders affordably, second; by advising governments, health institutions and all stakeholders about the best approaches to ensue the efficiency of health care services’ provision.
This will enable access to improved health-related services and hence reducing the delay to patients receiving health care.
Additionally there will be improved clinical outcomes, such as reduced infant mortality, longer life-spans and decreased contraction of diseases.